One of the most challenging and divisive decisions of the coronavirus pandemic is whether and how to reopen schools this fall.
We heard the same thing from a dozen nationally prominent psychologists, parenting experts and authors with whom we met by Zoom recently. One after another admitted that they, too, were unsure what they will do for their own children.
“We want our children to return to school for a variety of reasons, but safety is our top priority right now,” says Katie Hurley, a child and adolescent psychotherapist.
If experts aren’t sure what to do, how should parents decide?
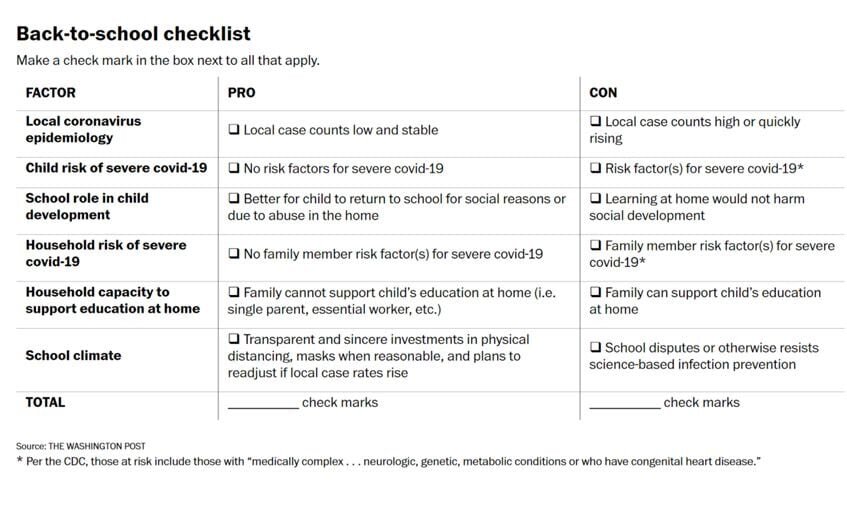
In a new story in The Washington Post, co-written with the esteemed (and I would say beloved) parenting author Jessica Lahey, we summarize the data pro and con returning kids to school and provide a decision-making checklist to help parents make the right call for their own families.
The quick summary is that there is no one-size-fits-all answer, and parents and schools need to individualize decisions based on local epidemiology, family health issues, and how seriously schools take science-based prevention. Here’s a tweetorial.

![[ M U R M U R S ]](http://images.squarespace-cdn.com/content/v1/51efa33ce4b09afa04cb2a66/1376911411704-LDY4UEIH1WRGPUXTMLJU/Logo.jpg?format=1500w)